NIH grant funds research to stop multiple myeloma at its source
NIH grant funds research to stop multiple myeloma at its source
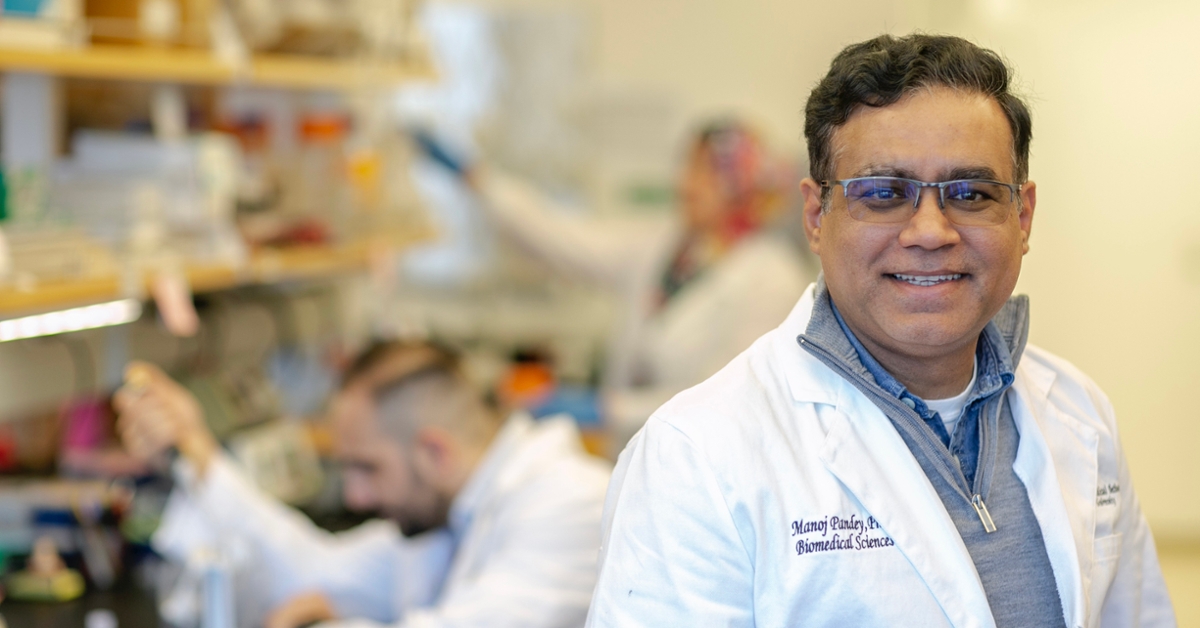
Manoj Pandey, Ph.D., an associate professor in the Department of Biomedical Sciences at Cooper Medical School of Rowan University (CMSRU), has received a four-year grant for $644,000 from the National Institutes of Health (NIH) to investigate the potential use of a new experimental compound against the incurable blood cancer multiple myeloma. The work is supported by nearly eight years of research at Rowan.
Multiple myeloma arises in the bone marrow, when plasma cells, a type of immune cell, become malignant. The risk increases with age, and most cases are diagnosed in people 55 or older. Patients are, on average, about 58 percent as likely as people without multiple myeloma to survive for five years.
“Multiple myeloma is a very challenging disease,” Pandey said. “Even under the best possible conditions, if you treat it with the best possible tools, every single patient will relapse and develop resistance to treatment over time.”
Pandey’s research focuses on the source of relapses: a population of cancer cells known as stem-like cells. Stem-like cells drive cancer by proliferating to produce malignant plasma cells. Even if treatment eradicates the malignant plasma cells, cancerous stem-like cells remain to seed a relapse, likely with the new ability to thwart the treatment the patient received previously.
Studies have shown that these cells produce unusually large amounts of the enzyme aldehyde dehydrogenases, known as ALDH, the composition of which can vary. Bortezomib, typically the first treatment given for multiple myeloma, can eradicate the cancerous plasma cells. However, ALDH in the stem-like cells can neutralize the drug, setting the patient up for a relapse.
While ALDH inhibitors are available, they cannot simultaneously target enough forms of ALDH to effectively interfere with the cancerous stem-like cells. Pandey’s group has developed a molecule, called KS100, which inhibits many different forms of ALDH.
In previous experiments with cells and mice, researchers combined bortezomib with KS100. They found that this combination killed off 99 percent of stem-like cancer cells.
With the NIH funding, the researchers plan to continue testing KS100 alongside bortezomib and other cancer drugs. They will apply these combinations to treatment-resistant stem-like cells grown in the lab, to cells derived from human patients, and in mice.
Their experiments will also explore a poorly understood racial disparity in multiple myeloma: Black patients are more than twice as likely to develop this cancer as their white counterparts. When patient samples are collected, participants will designate a race, and Pandey plans to use this information to investigate whether differences in ALDH somehow contribute to the disparity.
In addition, he plans to study how KS100 behaves in the body, studies that could help lay the groundwork for developing it as a drug to either prevent multiple myeloma from developing in the first place or at least slow its progression.
Rowan’s Ph.D. programs in pharmaceutical chemistry and in molecular cell biology and neuroscience have proven essential to this research. Robert Chitren, who conducted the preliminary experiments, was a Ph.D. student in the pharmaceutical chemistry program.
“His work led to the NIH funding for this project,” Pandey said. Chitren has since graduated, so the grant will support another student, this time from the new molecular cell biology and neuroscience doctoral program, who will take over the project.
Rowan’s investment in the Ph.D. programs is now paying off, he said. “These students are working hard, and they’re helping principal investigators to generate data on clinically important projects.”