NIH grant puts Rowan stroke intervention one step closer to patient-ready device
NIH grant puts Rowan stroke intervention one step closer to patient-ready device
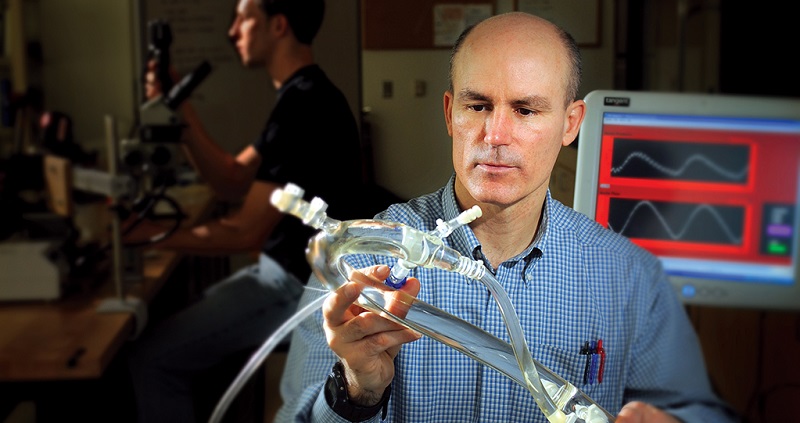
In the lab at medical device startup FocalCool, a sprawling collection of tubes and valves represents the cardiovascular system. Dr. Tom Merrill, associate professor of mechanical engineering at Rowan University and CEO and co-founder of FocalCool, uses this test-rig patient to design and refine an innovative catheter-based cooling technology that could save the lives—and preserve the brain function—of stroke patients.
This promising new technology, named Khione after the Greek goddess of snow, earned FocalCool a nearly $2 million grant from the National Institute of Neurological Disorders and Stroke, part of the National Institutes of Health.
“Stroke is consistently one of the top five leading causes of death and the number-one leading cause of serious disability, with 800,000 in total and 600,000 first strokes happening each year in the United States,” said Merrill, a professor in the Henry M. Rowan College of Engineering.
His innovation could help ischemic stroke victims, which account for 80 percent of all strokes. And this two-year, phase-two grant is exactly what’s needed to take the project from a pre-clinical prototype to a patient-ready, FDA-level device capable of saving lives.
Turning hypothermia into a medical treatment
Most people equate hypothermia with being trapped in sub-zero temperatures and freezing, if not to death, then into a state of unconsciousness.
What happens in therapeutic hypothermia – intentionally induced in a hospital – is similar to what occurs when someone suffers hypothermia in freezing temperatures.
As whole-body temperature lowers, the body’s functions slow down. This slowdown can actually help minimize the damage that transpires when the brain is deprived of oxygen. Breathing and heart rate slow under hypothermic conditions, and the cells that would otherwise die off at rapid rates without oxygen now – temporarily – require less blood flow.
In particular, therapeutic hypothermia helps prevent damage from a condition called ischemia reperfusion (IR) injury. Ischemia occurs when a blood clot restricts blood supply, depriving the brain of oxygen. Restoring blood flow is crucial to preserving patients’ lives and function, but in this process of reperfusion, additional tissue damage can occur. The mechanism of this damage is another function slowed by hypothermia.
In these not-so-rare cases – hundreds of thousands of which occur each year – hypothermia isn’t life-threatening, but lifesaving.
Doing in minutes what once took hours
How neurointerventionists get brain tissues in danger of damage during a stroke down to hypothermic temperatures makes a difference. Lowering the temperature of the entire body isn’t ideal.
“If you cool the whole body, it reacts in an evolutionary way,” said Merrill. There’s an involuntary shivering effect. Under systemic hypothermia, wounds – including those necessary for medical intervention – don’t heal as well. And the temperature of the body affects the rate at which drugs behave in the bloodstream, altering how well they work.
Perhaps even more importantly, it takes a long time – precious time stroke victims don’t have.
“In a stroke, time is your enemy,” Merrill said. “Nearly two million neurons die per minute when stroke goes untreated.”
Lowering whole-body temperature takes hours. But what if doctors could cool only the brain – or better yet, only the parts of the brain most at risk – in just a fraction of the time?
“We call it rapid selective cooling,” Merrill said of the innovation that sets FocalCool’s work apart. “Focusing on an organ or part of an organ allows you to cool more rapidly and get the tissue in danger to a protected temperature with less lag time.”
Rapid selective cooling doesn’t just avoid those side effects of whole-body cooling. It can shorten the cooling process from multiple hours to a span of just 5 to 10 minutes – preserving billions of a patient’s brain cells.
Progressing to a patient-ready device
FocalCool’s work is part of a revolution involving mechanical intervention. It’s not chemical-based, but device-based.
In mechanical intervention, doctors use minimally invasive procedures to insert a series of catheters and interventional devices – like a shape memory material that, under the right conditions, expands into a cage large enough to fully engulf the clot causing the stroke.
It may sound like something out of science fiction, but, Merrill said, “this ‘science fiction’ is saving lives.” In fact, he said, data show that a stunning 45 percent of patients treated with this procedure, called mechanical thrombectomy, achieved independence within 90 days of a stroke.
FocalCool’s localized therapeutic hypothermia technology could make procedures like this even more effective by pre-cooling – inducing organ hypothermia even before bringing in this series of catheters – and then maintaining the low temperature after catheterization to minimize the damage from reperfusion injuries.
The patient-ready device doesn’t exist just yet. But Merrill and his team are working to make it a reality.
“We have prototypes, but we’re still in the pre-clinical stage,” Merrill said. “The clinical studies needed to demonstrate the device is effective are remarkably expensive.”
The initial results of pre-clinical work were promising indicators that the device will be safe and effective. Now, this phase-two grant will enable Merrill’s team to develop the patient-ready device.
“At the end of this project, we aim to have an FDA-approved device,” he said. “To help the most patients, we need three elements: an FDA-approved device, successful clinical trials, and a successful marketing campaign to catch the attention of neurointerventionalists.”
Innovating interventions in hearts and minds
FocalCool has already developed localized therapeutic hypothermia catheters to treat heart attacks, but the company isn’t branching out into a new area. Rather, it’s the opposite.
“We began thinking of cooling the brain, but that proved unsuccessful with early devices,” said Merrill. “It was always in the back of our heads that we could improve our design and get back to brain cooling.”
Although both heart attacks and strokes involve blockages, there are crucial differences that made mechanical intervention more challenging in the brain.
“The heart is more robust, while the vessels in the brain are more delicate,” Merrill explained. “One is a complex and beautiful muscle. The other is the essence of who we are.”
In addition, there’s a more extensive history of innovation in mechanical intervention treatments, like angioplasty, for heart attacks than for strokes.
“Most people would consider a neurological intervention significantly more risky than cardiovascular intervention,” Merrill said.
In the finance world, too, a project like FocalCool’s seems risky. Medical device development is far from a sure investment, which often makes it difficult for teams like Merrill’s to find private investors, especially in early stages.
“We’re very grateful for this opportunity and that Rowan has supported this adventure,” said Merrill. In particular, he noted the level of support FocalCool has received from Provost Anthony M. Lowman and Jeanne Nevelos, managing director of Rowan Innovations and executive director of the South Jersey Technology Park, where the startup’s lab is located.
More than 30 students have worked in FocalCool’s lab since 2008. Although Merrill is currently on sabbatical from teaching to concentrate on his work with FocalCool, he continues to inspire students in the lab.
“Working with Dr. Merrill has majorly impacted me as an engineer,” said Jennifer Poff, 23, a senior mechanical engineering major from Barrington. During the Fall 2019 semester, Poff used computer-aided design software SolidWorks to create a 3D video production FocalCool could share with investors, neurointerventionalists and the FDA.
“I was able to improve not only in SolidWorks but also with communication and problem solving,” Poff said. “This project has also given me a tangible video that I can use at future events to showcase my SolidWorks abilities.”
Merrill’s former clinic student Michael Vigilante, 22, of Washington Township, recently accepted a post as FocalCool Research and Development Engineer.
“One of the most important things I have learned when working with FocalCool is how to go through the engineering design process to attain a successful project,” said Vigilante, who graduated last year with his degree in mechanical engineering. “Understanding the engineering design process provides a route to success when dealing with a forest of obstacles to overcome.”
By realistically simulating a professional work environment, Vigilante noted, Merrill’s clinic course also prepared him and his fellow engineering students to transition into real-world work environments.
“I gained a real comparative experience of how engineering is conducted when a student eventually becomes a professional,” Vigilante said. “Going through the clinic experience with FocalCool has helped me become a better engineer.”
FocalCool has come a long way since Merrill launched the startup in his basement. But the company still has a long way to go – and plenty of inspiration to stay on track.
“This hand shook Henry Rowan’s hand, and I take that very seriously,” said Merrill. “He would want us to work very hard, with passion, to help people.”